U-M researchers decode steps in stem cells’ complex decision-making process

When a stem cell divides, the two new cells have to make some big choices, and fast. New research from the University of Michigan Life Sciences Institute has elucidated just how complex that decision-making process is.
In a new study, published November 21 in Genes & Development, U-M researchers shed new light on the mechanisms by which one of the new cells permanently sheds its identity as a stem cell. The findings could also point toward new approaches to getting tumor cells to likewise turn off their runaway replication.
Stem cells have the potential to develop into any type of cells that specific tissues within the body might need. When you have a cut, for example, stem cells can create new skin cells to help heal the wound. They do this by dividing into two different types of cells: one exact copy of the stem cell (to maintain the stem cell pool), and one that can become a new type of cell for a specific tissue.
“The cell that is going to start to differentiate has a lot of things to do,” explains Cheng-Yu Lee, Ph.D., associate professor at the LSI and senior author on the study. “It has to completely erase all stem cell signatures that it inherited so it does not assume a stem cell identity. It’s a critical commitment to make, and it has to be made quickly.”
If a cell can turn off all levels of the gene activities that tell it to be a stem cell, it will no longer make the messenger RNA (or mRNA for short) and proteins that maintain its stem cell identity.
The first step in turning on or off gene expression is called transcription, and controls the production of new mRNAs that encode proteins. Turning off stemness gene transcription will terminate the synthesis of new mRNAs that encode stem cell-specific proteins in differentiating stem cell progeny. However, this control mechanism alone is not sufficient to stop the production of new stem cell-specific proteins and inactivate those that already exist in the cell. To commit to differentiate, a stem cell progeny still has to rid itself of the stem cell-specific mRNAs and proteins that it already inherited from the mother stem cell.
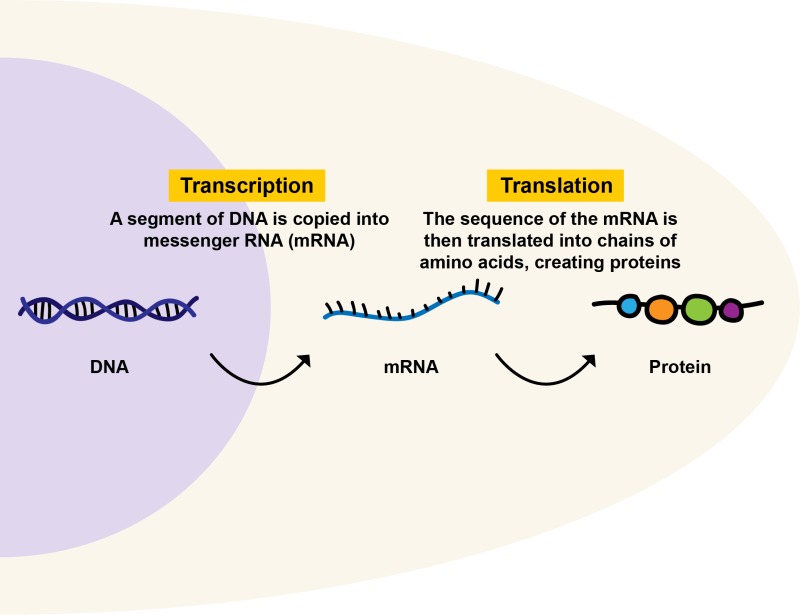
“In the scientific literature, there’s a huge emphasis on regulation of transcription for this process,” says Lee, who is also an associate professor of internal medicine and cell and developmental biology at the U-M Medical School. “But what we’ve come to realize is we need to think about it in a much more multi-dimensional way. In order for this transition to happen in a timely manner, multiple layers of controlled mechanisms must be working together.”
Using the model system Drosophila melanogaster, or fruit flies, the researchers identified two proteins that work together to prioritize the stem cell-specific mRNAs for destruction. They recognize a specific signature on these mRNAs and mark them as high-priority targets, so the RNA disposal machinery can quickly come in and degrade them.
A similar process occurs for any of the related proteins still hanging around as remnants of the original stem cell. The researchers found at least two cellular mechanisms working together to identify and destroy any proteins that function as stem cell factors.
Lee’s findings help unravel a complex process that is essential for the body’s ability to maintain and create the cells it needs for survival; and they have implications for cancer cell growth, as well.
Tumor stem cells and healthy stem cells share many functional characteristics. Lee believes that the same mechanisms that drive stem cells to differentiate could also drive tumor stem cells to give up their stemness properties and commit to differentiation instead. Determining how this process works could eventually open new doors to reducing tumor growth and relapse by shrinking the pool of tumor stem cells.
This new study demonstrates how multifaceted and complex that process is.
“The key thing here is that, conceptually, we need to think about transcription, translation, and post-translational regulation,” Lee says. “All of these mechanisms matter — and, in fact, they all have to work together to ensure this transition happens.”
Go to Article
Multi-layered gene control drives timely exit from the stem cell state in uncommitted progenitors during Drosophila asymmetric neural stem cell division, Genes & Development. DOI: 10.1101/gad.320333.118